The presence of an inflammation of the upper airways induced by the repeated airflow turbulence following the mechanical obstruction already has been demonstrated in sleep apnea subjects, as evidenced by increased concentrations of the inflammatory cytokine interleukin in exhaled condensate, and could be responsible for the generation of increased 8-isoprostane concentrations at the luminal surface. 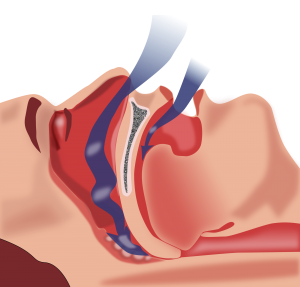
It is possible that the increased oxidative stress found systematically in OSA is a consequence of this local airway inflammation due to the mechanical injury. This could then account for the positive correlation we found between 8-isoprostane concentrations in the exhaled breath condensate and in the plasma of OSA subjects.
Although the precise cellular source of ROS in the upper airway is unknown, Saul et al showed that inflammation is present in the soft palate of patients with OSA. Furthermore, Zakkar et al demonstrated a decrease in the concentration of neutral endopep-tidase (which cleaves proinflammatory peptides) in the uvula of patients with OSA compared to control subjects. It has been suggested that an imbalance between oxidants and antioxidants may lead to atherogenesis, and that this may account for the several chronic cardiovascular complications that frequently are related to OSA.
In confirmation of our previous results, we observed a positive correlation between morning exhaled 8-isoprostane concentrations and neck circumference, suggesting that the measurement of exhaled oxidative stress markers may be useful in screening obese subjects who are at high risk of developing sleep apnea and in monitoring the progression of this syndrome.
The lack of correlation of exhaled 8-isoprostane concentration with the percentage of TST oxyhemoglobin saturation at < 90% and ODI, in contrast to the positive correlation observed with AHI, argues against a role for hypoxia as a possible causative factor of the increase of the oxidative stress. However, it is possible that there could be a relationship between 8-isoprostane and the number of oxygen desaturation episodes, rather than their severity.
In the present study, we repeated measurements of exhaled 8-isoprostane levels in OSA subjects before sleeping (ie, 8:00 pm) and at waking (8:00 am), observing higher levels of this marker at 8:00 am but observing their reduction after 12 h of being awake. These findings are consistent with previous observations, according to which the nocturnal apneas, through repeated hypoxia as a result of the mechanic obstruction, could be responsible for oxidative stress in patients with moderate-to-severe OSA.
Comments are closed, but trackbacks and pingbacks are open.